There are over 31 million cases of Sinus infection annually (called “rhinosinusitis (RS)” because both nose and sinuses are involved. Over 25 million office visits have been generated each year in the U.S. because of acute sinusitis, resulting in Expenditures of over $3 Billion on acute bacterial sinusitis. Acute sinusitis is most often preceded by a viral upper respiratory infection and it is felt that 2% of URI’s go into sinusitis. It can lead to asthmatic exacerbations and chronic headaches.
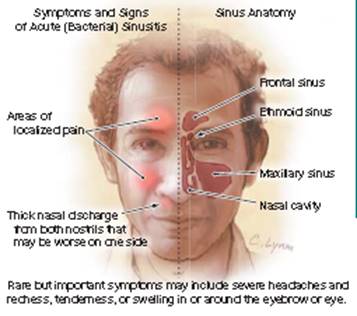
Signs of acute sinusitis include yellow mucus from the nose, nasal obstruction, facial or sinus pain, headache, and post-nasal drip all not improving over 10 days. Shown in the picture are the frontal sinuses, ethmoid sinuses (alongside the nose), Maxillary sinuses (in the cheeks) and not shown, the sphenoid sinus, deep in the center of the head.
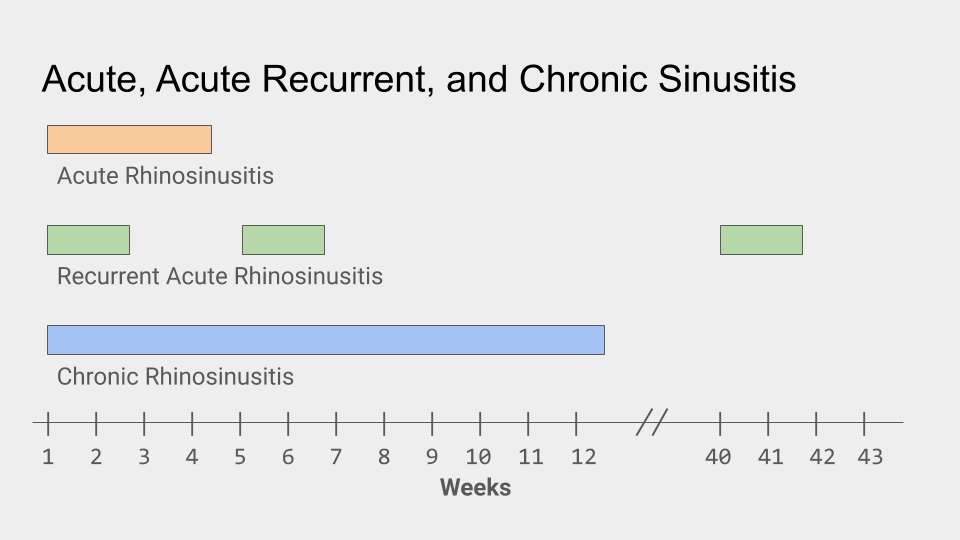
In acute sinusitis (RS), the sinus infection occurs once, and then the mucus membranes return to normal. In recurrent acute sinusitis, the infection seems to be over, but then the acute infection recurs. In between infections, sinus or CT of sinuses are normal.
In chronic RS, the mucus membranes are never completely normal between infections. Acute recurrent sinusitis and chronic RS may be associated with allergic disease, with the allergies causing obstruction and more infection.
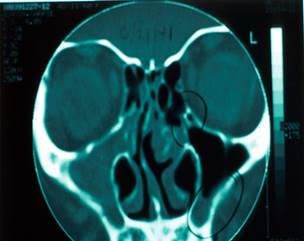
The pathology of sinusitis seems to be obstruction of the normal openings into the sinuses, called the ostiomeatal complex, with fluid accumulation and pus behind it. The normal ciliary action of the sinuses is missing or less than normal leading to fluid accumulation and sinus infection.
In this CT scan of the sinuses, one can see on one side the maxillary sinus is filled with mucus and pus. On the other side (marked by blackcircles) there is obstruction above leading to fluid accumulation below.
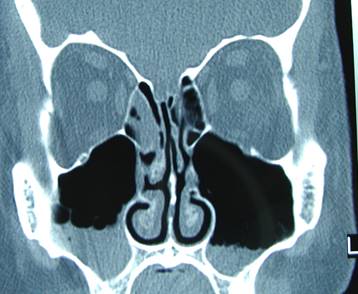
Chronic sinusitis is different from acute sinusitis. Often there was no acute sinusitis beforehand. Symptoms may be quite vague and pain or pressure may not localize well to each sinus. Cultures of sinus aspirates are often negative. On CT scan of the sinuses, there may be extensive mucus membrane thickening.

This is a much different picture on CT than acute sinusitis, which often starts in the ethmoids and drips into the maxillaries.
If a 10 day course of some common antibiotics (amoxicillin/clavulanate, doxycycline and rarely levofloxacin or moxifloxacin in adults-levofloxacin and moxifloxacin (now considered alternative antibiotics to be used rarely because of side effects)) or (amoxicillin, amoxicillin/clavulanate, or a cephalosporin in children) is not helpful, evaluation by ENT/allergy is probably indicated. Often an Allergist will start by taking a comprehensive history and doing a careful physical exam, getting a CT sinuses to confirm sinus infection, and performing skin tests to evaluate for allergies. He/she will treat with antibiotics and nasal sprays including nasal steroids. and other medications and even allergy shots. If these do not help, referral to an ENT specialist for evaluation for possible endoscopic sinus surgery may be indicated.
Clearing out the inflammatory material in the sinuses by surgery will often restore patient’s sense of smell. This may end the severe nasal obstruction that may be present resulting in better sleep. Sinus surgery is often necessary to get the disease process under control, and prevent recurrent infections. Surgery may also improve asthma by preventing infected mucus from dripping into the lungs. I must emphasize that not all sinus surgeons are of equal skill, and I would use one who I know by experience is highly skilled, talented, and has a history of good outcomes.