“Allergy Shots” (Allergen Immunotherapy) for Nasal Allergies, Asthma, and Stinging Insect Allergy
If you have allergies, you may be wondering if allergy shots are the best treatment for you. After all, getting regular shots isn’t anyone’s idea of fun, but the possibility of being free from your allergy symptoms may be worth it.
Allergies are the result of a chain reaction that starts in the immune system. Your immune system controls how your body defends itself. For instance, if you have an allergy to pollen, your immune system identifies pollen as an invader or allergen. Your immune system overreacts by producing antibodies called Immunoglobulin E (IgE). These antibodies travel to cells that release chemicals, causing an allergic reaction.
Allergy Shots (Allergy Immunotherapy)
Immunotherapy is a preventive treatment for allergic reactions to substances such as grass pollens, house dust mites and bee venom. Immunotherapy involves giving gradually increasing doses of the substance, or allergen, to which the person is allergic. The incremental increases of the allergen cause the immune system to become less sensitive to the substance, probably by causing production of a “blocking” antibody, which reduces the symptoms of allergy when the substances is encountered in the future. Immunotherapy also reduces the inflammation that characterizes rhinitis and asthma.
Before starting treatment, the physician and patient identify trigger factors for allergic symptoms. Skin or sometimes blood tests are performed to confirm the specific allergens to which the person has antibodies. Immunotherapy is usually recommended only if the person seems to be selectively sensitive to several allergens.
How allergy immunotherapy is done
An extract of a small amount of the allergen is injected into the subcutaneous tissue of the arm. An injection may be given once a week (sometimes more often) for about 30 weeks, after which injections can be administered every two weeks. Eventually, injections can be given every four weeks.
Who Can Be Treated with Shots?
Allergy shots are recommended for patients with allergic asthma, allergic rhinitis/conjunctivitis and stinging insect allergy. They are not recommended for food allergies. Before a decision is made to begin allergy shots, the following issues must be considered:
- Length of allergy season and the severity of your symptoms
- Whether medications and/or changes to your environment can control your allergy symptoms
- Your desire to avoid long-term medication use
- Time: immunotherapy requires a major time commitment
- Cost: may vary depending on your region and insurance coverage
Immunotherapy for children is effective and often well tolerated. It might prevent the onset of new allergen sensitivities or the progression to asthma.
In some patients suffering from other medical conditions or who take certain common medications, allergy shots may be more risky. It is important to mention other medications you take to your allergist.
Who Should Be Giving Allergy Shots?
Because adverse reactions to allergy shots may occur, your allergist has the right staff and equipment to identify and treat these reactions. If possible, allergy shots should be given in your allergist’s office. If not, your allergist should provide the supervising physician with complete instructions about your treatment.
How Do Allergy Shots Work?
Allergy shots work like a vaccine. Your body responds to the injected amounts of a particular allergen (given in gradually increasing doses) little by little, developing a resistance and tolerance to it. Allergy shots can lead to decreased, minimal or no allergy symptoms when you are again exposed to the allergen(s) in the shot.
There generally are two phases to immunotherapy: build-up and maintenance.
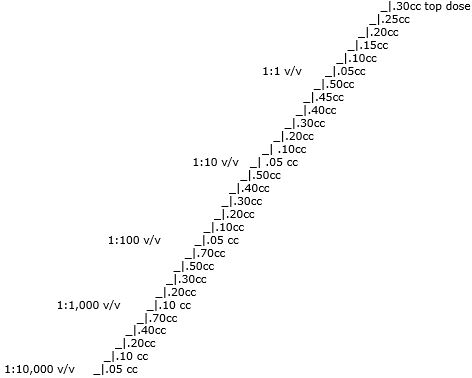
There may be more doses at 1:10 level and 1:1 level than shown. (There is now a new nomenclature for shots, listed as “v/v.”)
The build-up phase, as shown above, generally ranging from three to six months, involves receiving injections with increasing amounts of the allergens. The frequency of injections is once or twice a week, though more rapid build-up schedules are sometimes used. There may be a few more doses at higher levels than shown in the diagram depending on time of year and if you have reactions to the shots.
The maintenance phase begins when the most effective dose is reached. This dose is different for each person, depending on how allergic you are and your response to the build-up phase. Once the maintenance dose is reached, there are longer periods between injections, typically two to four weeks.
When Will I Feel Better?
For some people, a decrease in symptoms is seen during the build-up phase; for others, it may take as long as 12 months on the maintenance dose.
If you don’t respond, it may be caused by:
- Not enough dose of the allergen in your vaccine
- Missing allergens not identified during your allergy testing
- High levels of the allergen in your environment
- Major exposure to non-allergic triggers (i.e. tobacco smoke)
If there is no improvement after a year of maintenance allergy shots, your allergist will discuss other treatment options with you.
When Should Allergy Shots be Stopped?
Once the maintenance dose is reached, effective immunotherapy is generally continued for three to five years. The decision to stop should be discussed with your allergist at that time. Some individuals may experience a permanent reduction of their allergy symptoms but others may relapse and a longer course of allergy shots can be considered.
What Are the Possible Reactions?
Immunotherapy, provided by qualified physicians, is an effective and safe treatment for asthma, allergic rhinitis and insect venom allergy. There are two types of adverse reactions that occur with allergy shots. Local reactions are fairly common and occur as redness and swelling at the injection site. This can happen immediately, or several hours after the treatment. Systemic reactions are much less common, are usually mild and typically respond quickly to medications. Signs include increased allergy symptoms such as sneezing, a stuffy nose or hives. Rarely, a serious systemic reaction called anaphylaxis (an-a-fi-LAK-sis) can develop, with swelling in the throat, wheezing, a feeling of tightness in the chest, nausea or dizziness.
Most serious systemic reactions develop within 30 minutes of allergy injections. This is why it is strongly recommended you wait in the office for 30 minutes after your injections. Since there is a small but real risk of severe reactions, allergy shots must be given in a doctor’s office where the physician is qualified and has the medication and tools to treat severe allergic reactions. Allergy shots may not be given at home in the absence of a doctor.
Your allergist is trained to watch for such reactions and his or her staff is trained and equipped with the proper medications to identify and treat them.
Healthy Tips
- Allergy shots are a treatment aimed at building up your tolerance to the substances that trigger your allergy symptoms.
- Allergy shots work like a vaccine. Your body begins to respond to the injected amounts of an allergen by developing resistance and tolerance to it.
- While most people may experience a permanent reduction of their allergy symptoms, others may not respond to allergy shots.
- An allergist can test you for allergies and tell you if allergy shots are right for you.
- Reactions are possible, but your allergist is trained to watch for them and his or her staff is trained to identify and treat them.
Effective treatment for asthma
A meta-analysis of 20 published prospective studies showed that allergen immunotherapy is effective in the treatment of asthma.(1) The American College of Allergy, Asthma & Immunology (ACAAI) recently compiled an annotated bibliography of 59 articles from the medical literature indicating the value of expert care and immunotherapy for asthma.(2) A meta-analysis of 23 published studies involving 935 asthmatic patients with documented allergy indicated that immunotherapy is effective in a selected population of allergic asthmatic patients.(3)
Effective treatment for allergic rhinitis
An extensive review of immunotherapy for allergic rhinitis in children showed that the only treatment able to affect the natural cause of the disease is immunotherapy, and that immunotherapy may prevent the onset of asthma.(4) A meta-analysis of 18 published studies involving 789 patients concluded that immunotherapy is highly effective in the treatment of allergic rhinitis.(5)
Effective treatment for insect venom allergy
Immunization with insect venom is an extremely effective treatment for preventing future systemic reactions to insect stings in individuals with previously demonstrated susceptibility.(6) A meta-analysis of nine published studies indicated that a course of immunotherapy is highly effective in the management of insect sting hypersensitivity.(7)
Immunotherapy safety
A report from the Mayo Clinic on 79,593 immunotherapy injections over a 10-year period showed the incidence of adverse reactions to be less than two-tenths of 1 percent (0.137 percent). Most of the reactions were mild and responded to immediate medical treatment. There were no fatalities.(8)
More than 1 million injections were given without a fatality to 8,706 patients in allergy clinics at Roosevelt Hospital, New York City, between 1935 and 1955.(9)
References
- Abramson MJ, Puv RM, Weiner JM. Allergen immunotherapy effective in asthma? A meta-analysis of randomized controlled trials. Am J Respir Crit Care Med 1995;151:969-974.
- Sullivan TJ, Selner JC, Patterson R, Portnoy J, Seligman M. Expert Care and Immunotherapy for Asthma. A review of published studies with emphasis on patient outcome and cost. ACAAI Monograph, Nov 1996,1-25.
- Ross RR. Effectiveness of immunotherapy in the management of asthma: A meta-analysis of the literature. May 1997. Data on file with American Academy of Allergy, Asthma & Immunology (AAAAI) and American College of Allergy, Asthma and Immunology (ACAAI) and submitted for publication.
- Bousquet J, Demoly P. Specific immunotherapy for allergic rhinitis in children. Allergy Clin Immunol Inter 1996; 8:145-150.
- Ross RR. Effectiveness of immunotherapy in management of allergic rhinitis: A meta-analysis of the literature. May 1997. Data on file with AAAAI and ACAAI and submitted for publication.
- Valentine MD. Anaphylaxis and stinging insect hypersensitivity. JAMA 1992; 268:2830-2833.
- Ross RR. Effectiveness of immunotherapy in the management of insect venom hypersensitivity: A meta-analysis of the literature. May 1997. Data on file with AAAAI and ACAAI and submitted for publication.
- Valyaservi MA, Yocum MW, Gosselin VA, Hunt LW. Systemic reactions to immunotherapy at the Mayo Clinic. J Allergy Clin Immunol 1997; 99:S66.
- Van Arsdel PP, Sherman WB. The risk of inducing constitutional reactions in allergic patients. J Allergy 1957; 28:251-261.